Imagine a world where your doctor and nurse lived in your community, or even on your street.
Your neighborhood provider has walk-in hours seven days a week. If you can’t make it in, the doctor and/or nurse will come to your house or place of employment to check on you there. Need a dentist, ultrasound or simple procedure? We have a clinic for that. Can’t make it to the clinic? We can bring the clinic staff to you. How will you afford it? All have health insurance for whatever care they need. Some people may say this sounds like a healthcare fairy tale.

However, this fairy tale is achievable and it is reality for the people of Cuba.
Make no mistake, Cuba is a ruggedly emerging nation, carved by a turbulent political history. The Cuba of today is a series of dichotomies wrapped in dappled layers of Havana’s retro chic.
I experienced all of this first hand with a group of 18 executives and leaders from around the United States. Our goal was to spend a week learning about the nuances of the Cuban healthcare system. Our group toured every aspect of care provided to the Cuban people, including education for their healthcare professionals.

Each person from our group represented different aspects of healthcare (academia, practice, industry, healthcare foundations, payors and even a member of the Federal Reserve) within the United States. For a week, we were able to pull out our inner anthropologists. Margaret Mead said, “anthropology demands the open-mindedness with which one must look and listen, record in astonishment and wonder that which one would not have been able to guess.” So, that’s exactly what we did.
Our group became fully immersed in the culture and were there just after the election of Cuba’s first President. Because of the flipped economics in Cuba, we learned it’s not uncommon for people with advanced degrees (mechanical engineers, architects, and PhDs) to work in the tourist industry. People working in the tourist industry can make 10 times more than a doctor. The average salary for a Cuban provider is $80/month; a nurse will make between $60-$70/ monthly. The health professionals we met work very hard to ensure their communities are developing and healthy
 Cuba’s national healthcare system ensures every citizen across the country has a healthcare evaluation and dental visit yearly. The average life expectancy for Cubans is the same as the United States. Herein lies a Cuban dichotomy, healthcare economics will tell you wealthy countries across the world tend to have better healthcare outcomes and ultimately the health of a population may impact the economics of a nation. Cuba can compete with some of the top developed nations around healthcare quality, and as a nation it has not allowed economic barriers to hinder its ability to deliver impressive healthcare outcomes.
Cuba’s national healthcare system ensures every citizen across the country has a healthcare evaluation and dental visit yearly. The average life expectancy for Cubans is the same as the United States. Herein lies a Cuban dichotomy, healthcare economics will tell you wealthy countries across the world tend to have better healthcare outcomes and ultimately the health of a population may impact the economics of a nation. Cuba can compete with some of the top developed nations around healthcare quality, and as a nation it has not allowed economic barriers to hinder its ability to deliver impressive healthcare outcomes.
Some underlying tenants of the Cuban healthcare system are captured in the Declaration of the Alma-Ata, a document created and ratified by Cuba during an international conference held in 1978 (excerpts below):
- Section I: Health, which is a state of complete physical, mental and social wellbeing, and not merely the absence of disease or infirmity, is a fundamental human right and that the attainment of the highest possible level of health is a most important world-wide social goal whose realization requires the action of many other social and economic sectors in addition to the health sector.
- Section IV: The people have the right and duty to participate individually and collectively in the planning and implementation of their healthcare.
- Section V: Governments have a responsibility for the health of their people which can be fulfilled only by the provision of adequate health and social measures. Primary healthcare is the key to attaining this target as a part of development in the spirit of social justice.
- Section VI: Primary Healthcare is the first level of contact for individuals, the family and community with the national health system bringing health care as close as possible to where people live and work.
- Section IX: All countries should cooperate in a spirit of partnership and service to ensure primary health care for all people since the attainment of health by people in any one country directly concerns and benefits every other country.

So, what’s the magic to Cuba’s system?
Without a doubt, it’s Cuba’s primary healthcare model and infrastructure, which address prevention and the social determinants of health. Cubans are evaluated by their provider yearly for factors related to lifestyle, environment or workplace risks and for any new or progressing disease. Cuban providers categorize people to determine disease stratification for their population, and to determine the number of times a patient will need to be seen over the course of a year, or if advanced testing or procedures are necessary. One of four categories is assigned to each person by a provider from a local consultorio:
- Group I: Perceived healthy individuals
- Group II: At-risk individuals (may develop health problems due to risk)
- Group III: Actively sick (chronic, communicable or non-communicable diseases)
- Group IV: Disabilities (temporary or permanent) including incapacitation related to a disturbance in motor, function, sensory or mental capability
 A consultorio serves multiple purposes, with their primary function being a medical resource location for each community. Each consultorio has a dedicated nurse and physician who live with their families on the second and third floor of the consultorio. Living within the community they serve gives the clinical team a deep understanding of what’s impacting their local population. A consultorio serves an area between 700-1500 residents. This physician/nurse team sees each resident yearly or more if necessary. The consultorio team also gathers health statistics and completes an epidemiological assessment for their residential area each year.
A consultorio serves multiple purposes, with their primary function being a medical resource location for each community. Each consultorio has a dedicated nurse and physician who live with their families on the second and third floor of the consultorio. Living within the community they serve gives the clinical team a deep understanding of what’s impacting their local population. A consultorio serves an area between 700-1500 residents. This physician/nurse team sees each resident yearly or more if necessary. The consultorio team also gathers health statistics and completes an epidemiological assessment for their residential area each year.
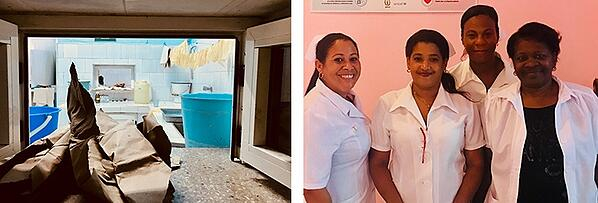
The first floor of the consultorio we visited had a small lobby with five chairs, which felt like a friendly public gathering point. The lobby led directly into a small room with a short metal desk and a green metal chair for patients, a small table, and a metal two-drawer filing cabinet. Hanging on the walls were a handmade poster board showing a map of an area that they were targeting for hygiene, a small lightbox, and a photo of Che Guevara. The metal file cabinet held all of the paper medical records for the people in their catchment area. A single file contained the health information for an entire family, because treating an individual meant understanding every aspect of their family’s health, including their social backgrounds.
The morning at the consultorio is busy with walk-in appointments. Afternoons are spent doing field work, where nurses and providers walk to patients’ homes and visit with people in the community. While out in the community, the care team is providing health promotion and screenings, patient health education and prevention, assessing community environmental factors and seeing individuals who may have difficulty getting to the clinic. If patients have complex care needs beyond what can be provided at the consultorio the provider will refer individuals to a polyclinica.
A polyclinica has a much larger service area of between 18,000-35,000 people. Like the consultorio, they use the provider and nurse team model for patient assessments. Polyclinicas provide immunizations, dental care, radiology, physical therapy, EKG and smaller surgical and procedural areas, as well as a pharmacy for controlled substances. Patient visits to a polyclinica are immediately reported back to the consultorio provider to ensure appropriate follow-up. If patients are unable get to a polyclinica, staff from the polyclinica will travel to a consultorio. The next level of care is more specialized, with institutes for diabetes, neurology, nephrology, etc., or admission to a general, pediatric, surgical or women’s hospital.
 We toured the Latin American School of Medicine (known by the Spanish acronym, ELAM). ELAM trains physicians for over 83 countries. They want their students to come from areas of high need, so they can go back to help those communities after graduation. The focus of their six-year medical model is health promotion, improving disparities, decreasing inequalities and the power of a strong patient historical exam. We spoke with a group of students studying there from the United States, one student shared the following story:
We toured the Latin American School of Medicine (known by the Spanish acronym, ELAM). ELAM trains physicians for over 83 countries. They want their students to come from areas of high need, so they can go back to help those communities after graduation. The focus of their six-year medical model is health promotion, improving disparities, decreasing inequalities and the power of a strong patient historical exam. We spoke with a group of students studying there from the United States, one student shared the following story:
“If I get an ‘A’ on a test, and someone else in my cohort gets an ‘F’, then I get an ‘F’. Students are taught that for one person to have knowledge and not share it, or being unaware of how others are doing, or not recognizing when someone is struggling, and stopping to help them – is reason for failure. We all have to succeed together!”
This story underscores the heart of the Cuban collective succinctly: to succeed alone is to fail.
Cuba’s healthcare system is facing its own struggles. Their country is doing an incredible amount to progress health with finite resources. A lot of the facilities we saw were working with very basic materials, rudimentary supplies and equipment – all heavily impacted by sanctions. Cuba can be a hard place to get around; transportation is a known area for healthcare access improvement. Cuban providers and healthcare professionals work incredibly hard. As a healthcare professional, the equity, humanity and whole person care across the Cuban healthcare system was deeply moving.
Multiple healthcare systems within the United States are trying to find more holistic models to address cost through quality initiatives and population health. We need to understand the best practices within our own country, and across the globe, to determine what will work best for the United States. No country has a perfect model, but there is magic in exploring existing models to test new ones.
Healthcare facilities across the country are proven economic engines for the communities in which they reside, but cost is the proverbial elephant in everyone’s waiting room. We also know zip codes are the best indicator of life expectancy in the United States – and they shouldn’t be. The expansion from economic engines to community health promotion is not that big of a leap.
How can we apply the lessons we learned from Cuba to our own healthcare system? We continue to use social, economic and environmental drivers to address health disparities through:
- Multi-sector engagement to improve population health
- Health promotion as a lever to address healthcare inequities
- Policies that support public health initiatives and address the social health determinants
- Reforming payment models to delivery systems
- Bringing care as close as possible to where people work and live
- Creating a humane way to empower people and personalizing care for every person
Let’s continue to build, and re-imagine the future of care and health within our own country.

Blog authored by Oriana Beaudet, former Vice President, Transformation for Array Advisors.

