Co-authored by Neil Carpenter, this article originally ran in the May/June 2020 issue of Medical Design + Construction
State of Affairs
Simply put, the U.S. is not yet out of the woods. While the curve is bending – with CMS even releasing guidelines for reopening hospitals to elective procedures – no vaccine has been released, and no proven treatment has been identified for COVID-19. Our nation could see another wave of cases, or even several of them.
Studying locations that have already endured the virus, such as New Rochelle, New York and Seattle, Washington will give health officials a roadmap for contending with new waves via containment zones and other measures. However, the effects of past mistakes will continue to reverberate through the healthcare system; once social distancing measures are abated, the curve will bend back. Thankfully, health systems are catching up on making beds and PPE available – the counterpoint to burnt-out physicians and a lack of mass testing.
Capacity Expansion on Facility, System and State Levels

From a medical construction and design perspective, the crux of the impact of our industry’s contribution has been capacity expansion within healthcare facilities and through the conversion of alternative assets. The following outlines the approach Array has taken with clients during this time.
Increasing Capacity at the Facility Level
The extent to which health systems can expand capacity in place varies widely, but before deciding how to make more room, all systems need to determine if they have the support requirements to match.
Our guidance to administrators has been to first establish a baseline understanding of existing bed capacity and staff resources, then assess support requirements, such as: the ability to add negative airflow either to units or individual units, how documentation will take place, PPE supply, infection prevention measures, monitoring requirements and communication protocols.
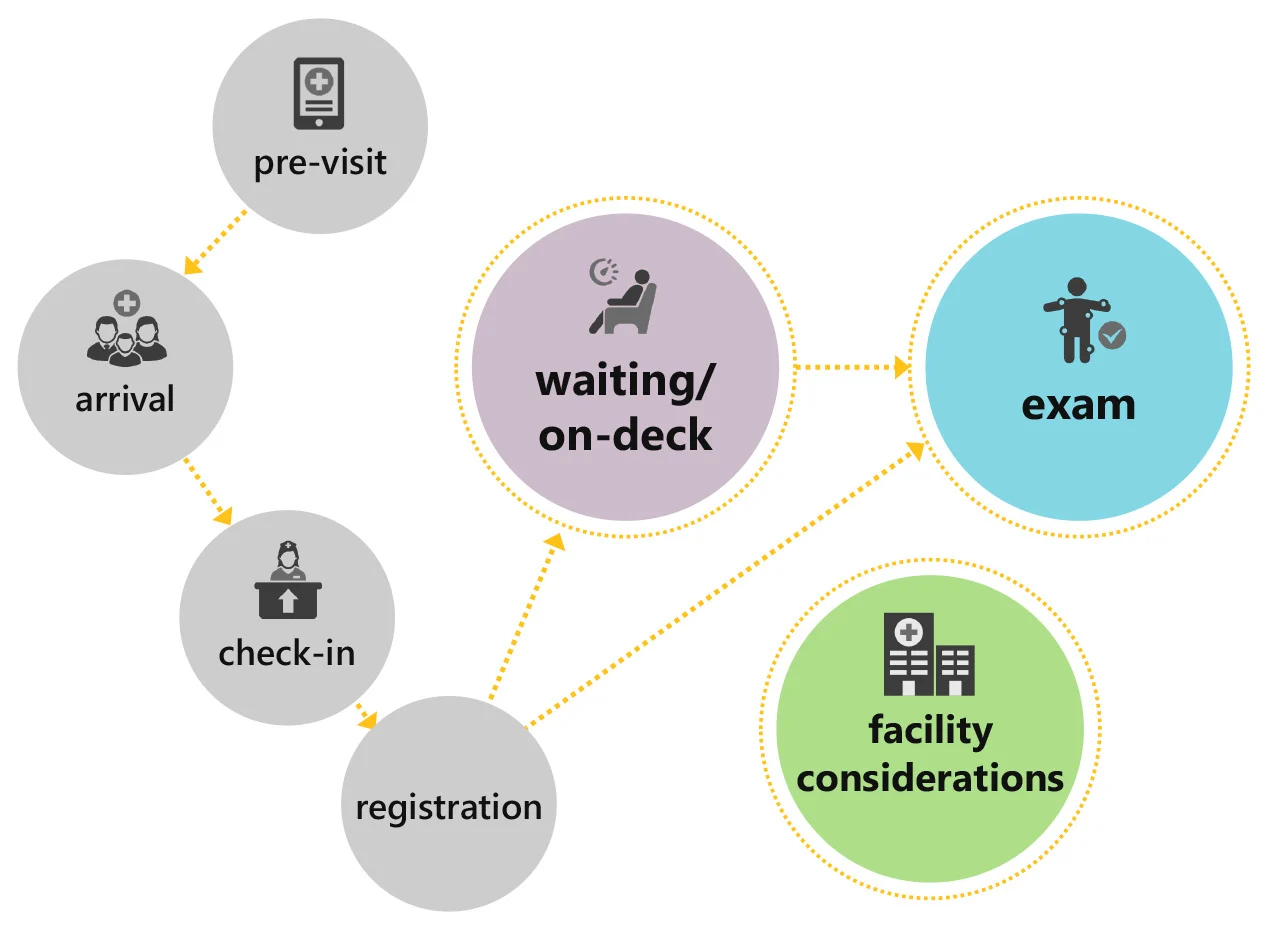
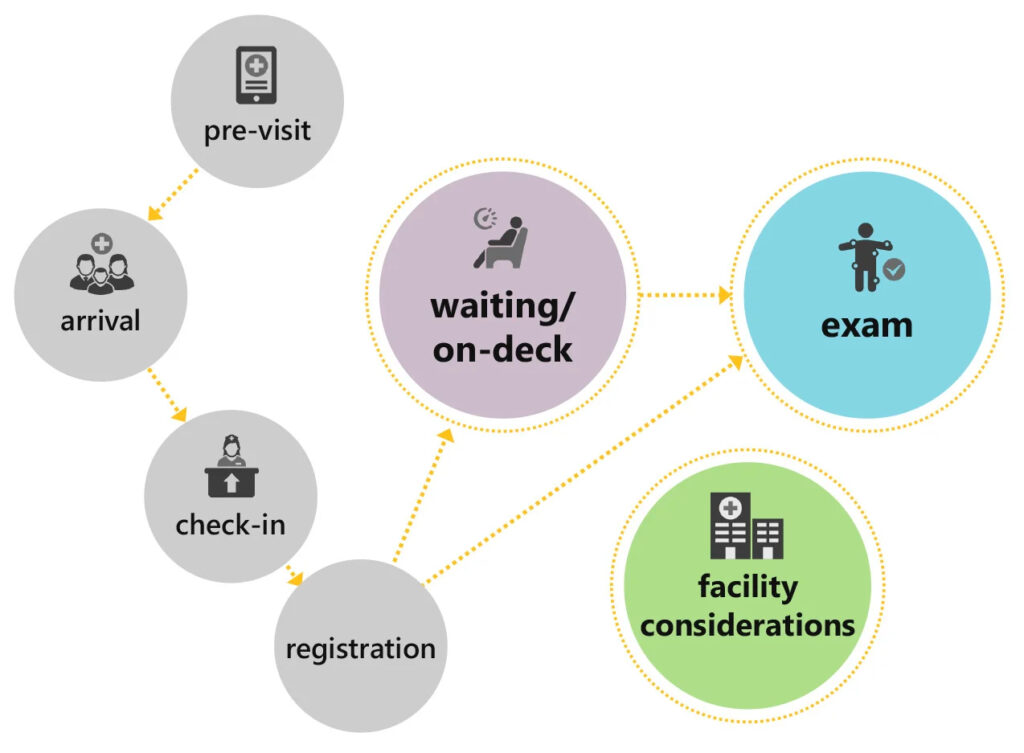
Once those factors are accounted for, planning for additional capacity requires an assessment of what the options for increasing capacity are and weighing them against the projected need. The need for additional space has an additional complicating factor: it is not just a need for more beds, but also segregated spaces to prevent further transmission at all points in the care continuum.
Many of our clients have created tent triage facilities outside of the ER for this purpose, but there is also a need to determine how patients will be segregated if admitted.
During the first month of the pandemic, many ideas were tossed around by the industry and the media on how hospitals and health systems could create more beds. Without a structured way to think through those options, some of the more extreme ideas, such as the use of hotels and convention centers, were gaining traction before other options were explored.
We guided our clients to consider capacity expansion options in tiers, from the most feasible to the more challenging.
In the first tier of options, we included recommendations to define and cancel elective surgeries, determine the feasibility of converting former semi-private rooms back to double occupancy, and to begin conversations with ASCs in the region to potentially leverage capacity.
If these steps alone did not create sufficient space to meet projected demand, we moved to a more rigorous review of assets: initiate the full capacity protocol, determine the feasibility of converting modern private rooms to double occupancy and assess capacity of prep/recovery spaces and alternate surgical recovery operational plans.
One client expanded their academic medical center by phasing capacity expansion. Starting with a baseline of 50 COVID-19 beds, over the course of four phases and with the conversion of PACU, observation units and the use of shelled space, the team was able to increase capacity to 362 beds. As a last resort, the system looked at using classrooms and portions of the ED – which would allow them to accommodate projected demand of 478 COVID-19 patients.
Increasing Capacity at the System Level
If tier one and two interventions were insufficient, we guided clients to consider coordinating more extreme solutions that leverage other facilities within their network or region. Those solutions include relocating hospital-based surgical and post-surgical services (and other cases not related to COVID-19) to an aligned ambulatory surgery center in their network, and creating OB delivery spaces in an MOB or even in temporary structures outside of hospitals or ASCs, where patients would be closer to higher-acuity care if their condition worsened.
Increasing Capacity at the State Level
Early Lessons from Preparing Non-traditional Sites of Care
Setting up alternative care sites is extremely resource-intensive and the spaces inherently limit the level of care that can be provided within them. Thus, these alternative sites are best used for non-COVID-19 patients or to divert COVID-19 patients whose condition is improving so that they can convalesce in a lower-acuity setting and free up hospital beds for others.
Modular units, convention centers and hotels are being used to treat or house COVID-19 patients across the nation. In particularly hard-hit areas, such as New York City, these unconventional care sites have been crucial to meeting demand, and FGI guidelines have loosened to allow their use.
 Our team worked with iCrowd and the New York State Department of Health to develop a design for five tent sites accommodating 1,000 COVID-19 patients in each. The plan specifies tents that use triage rooms with a one-way flow model to keep patients moving through the space, 400 double-bed bays and 200 isolation rooms. The tents would be equipped with centralized nursing stations with hand-washing sinks, full medical gases and electrical power, staff lounges throughout the central core and rapid response labs with point-of-care testing. Plans for these rapidly deployable structures demonstrate that it is possible to ease the burden placed on already-stressed hospital systems if demand exceeds the original plans to expand capacity.
Our team worked with iCrowd and the New York State Department of Health to develop a design for five tent sites accommodating 1,000 COVID-19 patients in each. The plan specifies tents that use triage rooms with a one-way flow model to keep patients moving through the space, 400 double-bed bays and 200 isolation rooms. The tents would be equipped with centralized nursing stations with hand-washing sinks, full medical gases and electrical power, staff lounges throughout the central core and rapid response labs with point-of-care testing. Plans for these rapidly deployable structures demonstrate that it is possible to ease the burden placed on already-stressed hospital systems if demand exceeds the original plans to expand capacity.
What’s Next?
In the short term (through the end of 2020), we anticipate more capacity expansion activity in different parts of the country as they respond to growing cases and projected demand, but are hopeful that through social distancing and stay-at-home orders, the need will not be as dire as the first wave and will likely focus on expanding capacity within hospitals. Unfortunately, that may not be the case if these restrictions are loosened. Recently, lockdown protests have emerged in pockets across the country as a minority demands a return to normalcy, despite the public health risk, and some states have started to scale back orders.
What will be the “new normal” in the long term? That is a question we expect the healthcare industry will debate heavily in the coming months, particularly at the intersection of design and construction – but nothing close to consensus has emerged, yet.
If one thing is clear at this point, it is the fact that the U.S. healthcare system has been designed, operationally and physically, to be lean and very good at providing tertiary and quaternary care, and thus not very flexible around capacity. The COVID-19 pandemic should cause us to rethink investments in many areas to better serve patients, while balancing the need for preparedness for the inevitable “next time.”
Watch our recent webinar for a deep dive into these issues:
Blog authored by Catherine Castillo, former strategic planner with Array Advisors.


